A lifeline of hope: Expanded bone marrow transplant unit opens
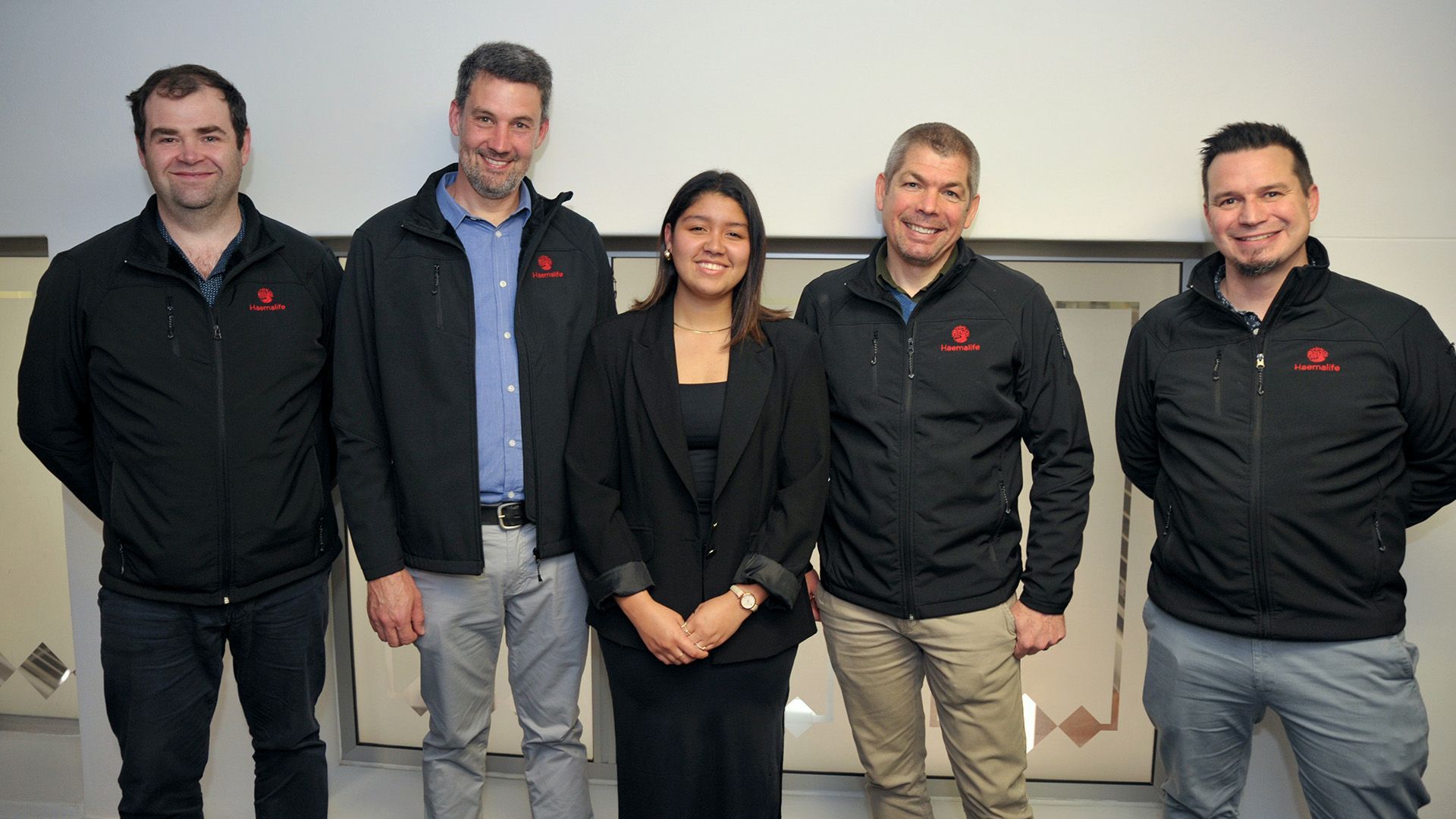
Haemalife doctors and Joy: (Left to right) Haematologists Dr Simon Brett, Dr Pieter de Witt, Dr Hannes Koornhof and Dr Michael Cass are pictured with Joy Schoor (centre) at the bone marrow transplant unit at Netcare Kuils River Hospital.
You could be someone’s one chance at life
For some people with life-threatening blood cancers, a bone marrow transplant may be their only remaining treatment option. The launch of the upgraded and expanded Haemalife Bone Marrow Transplant (BMT) unit at Netcare Kuils River Hospital signals more hope and an opportunity to create lifesaving awareness of South Africa’s bone marrow donor registry programmes.
“The time sensitive and highly specialised nature of haematology treatments, and the growing need for such services in the Northern suburbs of Cape Town and for patients from further afield, emphasises the importance of the additional capacity that has been created with this larger bone marrow transplant unit,” says Dirk Truter, general manager of Netcare Kuils River Hospital.
“We thank Dr Hannes Koornhof and Dr Pieter de Witt, the founding haematologists of the Haemalife practice, as well as their colleagues Dr Michael Cass, Dr Simon Brett, medical officer Dr Liza Stockland, and all members of this immensely caring team for their dedication to improving the facilities and growing the expertise available to help our patients and their families.”
Dr Koornhof says that the BMT Unit opened eight and a half years ago with eight beds and was very soon at full occupancy. The unit’s first of many successful bone marrow transplants was performed in February 2016.
“While the expansion of capacity is welcome news for patients who urgently need treatment and their referring doctors, there is also an urgent need for more South Africans to consider registering as potential bone marrow donors to contribute more diversity to the international bone marrow donor registry and increase the hope of finding suitable life-saving matches both at home and elsewhere in the world.”
“Specialised single isolation rooms, each with their own en suite bathroom and ventilation system, are required when a person has a bone marrow transplant or intensive chemotherapy,” adds Dr Cass.
“Before a bone marrow transplant, we need to suppress the person’s immune system with chemotherapy and specialised medications to reduce the risk of the patient’s body rejecting the introduced donated stem cells. For this reason, a very controlled environment is needed to protect the patient for three to six weeks,” he explains.
“With the Department of Health’s approval of the application, the BMT unit has now been expanded to 19 beds. The original isolation suites have been upgraded, and an upper level of isolation suites has been added on the floor above with an interlinking staircase, making this one of the largest bone marrow transplant units in the country.
“Bone marrow transplants may be indicated for leukaemia, multiple myeloma or lymphoma, or when a person’s body is unable to produce enough healthy blood cells due to a health condition or from the effects of prolonged treatment,” Dr De Witt says.
The Netcare Kuils River Hospital unit is the only facility in the northern suburbs to provide bone marrow transplants and treat acute leukaemia. Although adult patients are the focus, the unit also treats patients as young as ten years old. Holistic, personalised services are provided for all stages of treatment, including survivorship and palliative services that support the patient and their loved ones throughout.
The newest haematologist to join the multidisciplinary team, Dr Simon Brett, adds that some bone transplant patients may be able to receive a bone marrow stem cell donation from a family member if there is a close enough tissue match between them.
“For those who do not have a familial matching donor, there is only an average of one person out of every 100 000 tested who might be a compatible tissue match. The more people who register as bone marrow donors, the more patients with blood cancers or other blood disorders can be matched for a potentially lifesaving bone marrow transplant.”
Registering as a bone marrow donor is free of charge and non-invasive, and could save a life. For more information, please visit https://sabmr.co.za/become-a-donor/ and https://www.dkms-africa.org/get-involved/become-a-donor.
Contact the HaemaLife Bone Marrow Transplant Unit at Netcare Kuils River Hospital on 021 900 6277; via email reception@haemalife.co.za or visit https://haemalife.co.za/.
Leukaemia survivor returns as medical student
Bone marrow transplant inspired Joy’s career choice
Joy Schoor was just 14 when she was diagnosed with acute myeloid leukaemia. Now, celebrating eight years in remission, she is paying forward her second chance at life by studying to be a doctor and encouraging the public to join the registry of potential stem cell donors.
“I was returning with my parents from a holiday in the Kruger National Park when suddenly I started feeling sick and developed a fever. At first, doctors thought it could be a common infection and had to rule out malaria. After more tests at various hospitals, I was diagnosed on 10 January 2016 – although I didn’t fully understand what it meant at the time,” Joy, now 23, remembers.
“I have such a supportive family, and with my whole future in question, my parents heard that haematologists Dr Hannes Koornhof and Dr Pieter de Witt of Haemalife were equipped to offer the specialised bone marrow transplant procedure at the nearby Netcare Kuils River Hospital.”
As the first patient to receive a lifesaving bone marrow transplant at the hospital in 2016, it was a poignant moment when Joy was recently invited back as a guest of honour to cut the ribbon officially declaring the expanded comprehensive bone marrow transplant unit open alongside the haematologists who treated her then.
“My journey through three rounds of chemotherapy was not easy, but it is one of the reasons I was inspired to study to become a doctor. The warmth, compassion and kindness my family and I experienced at the unit during this difficult time in my teenage years stayed with me and made me want to help others in their time of need,” Joy says.
“Even though I was so young, the doctors explained everything so carefully to me and my parents and did everything they could to make us feel at home and as comfortable as possible in the circumstances.
“I am grateful that my brother, who was only 12 at the time, was an almost perfect tissue match and he agreed to donate stem cells to me for the bone marrow transplant I needed.
“There is only a 25% chance of a sibling being a match, and some people can have 12 brothers and sisters, and none of them are sufficient matches, so I was exceptionally lucky, and to this day can’t thank my brother enough – although he still teases me about it,” Joy says.
“Tragically, there are people in need of bone marrow transplants for whom matching donors can’t be found. As a survivor, this is why I would like to pay it forward by raising awareness of the need for more people to register as stem cell donors – you could save a life.”
Joy will also be job shadowing at the practice that saved her life as part of her medical studies later this year.
“I am making the most of my second chance at life, living my dream of becoming a healthcare professional and eight years cancer-free thanks to the specialised care I received here. I cannot tell you how significant it is for me to be cutting the ribbon at the same facility that will be a beacon of hope for many other families in the years to come,” Joy concludes.
Joy Schoor was the first patient to receive a lifesaving bone marrow transplant at the haematology unit at Netcare Kuils River Hospital in 2016.
Today Joy is studying to be a doctor herself and was recently invited to cut the ribbon at the launch of the expanded bone marrow transplant unit, where she is pictured with haematologist Dr Hannes Koornhof.
Dr Pieter de Witt, Joy and Dr Hannes Koornhof