Cochlear implant procedure now available at Netcare Kuils River Hospital
Patient’s hearing successfully restored, more to follow soon
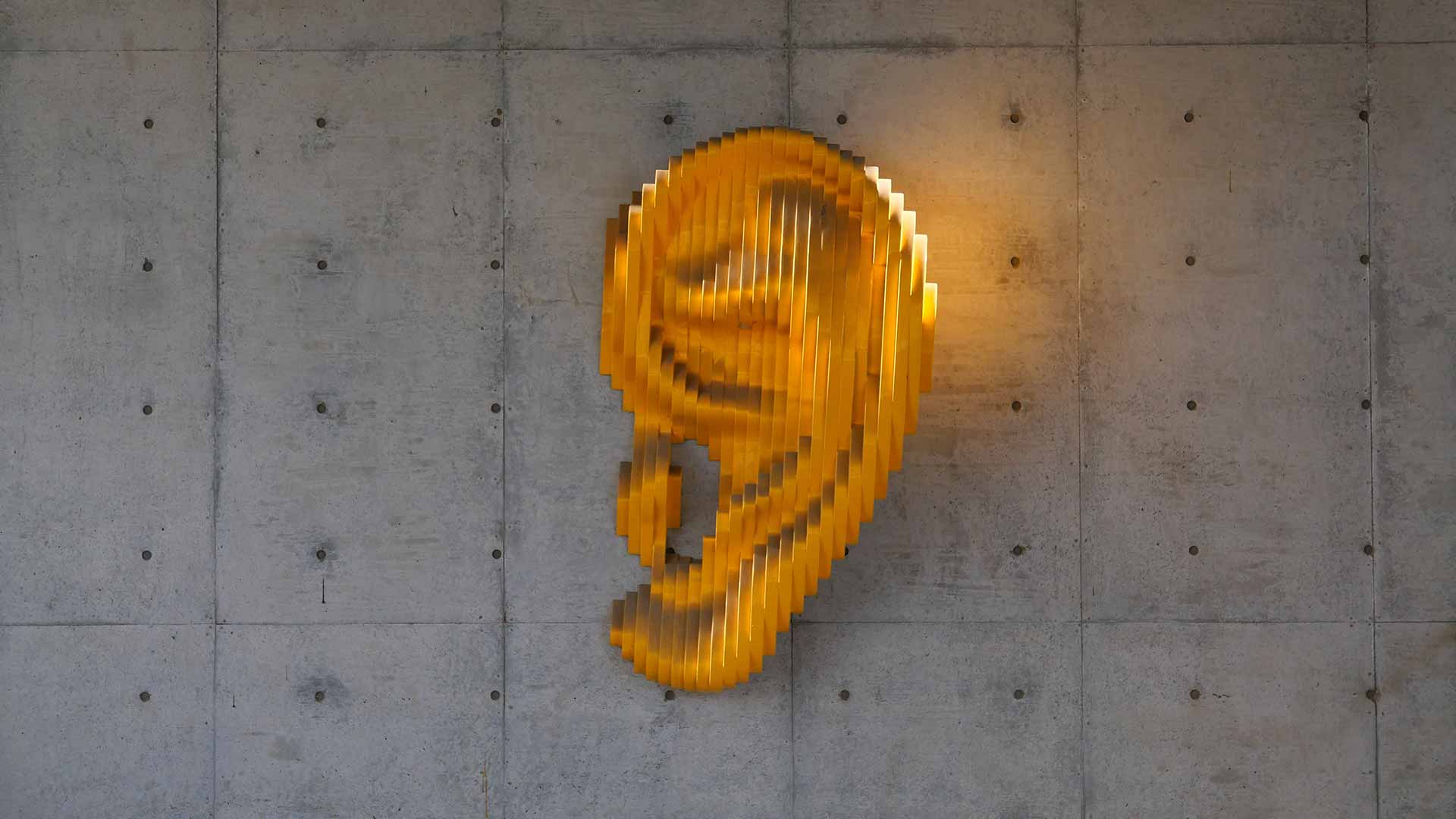
One of the five senses, hearing, allows us to listen to a favourite piece of music, become alerted to a ringing doorbell or hear another’s voice. Life without this sense can be productive and rich, however, there is a procedure – cochlear implant surgery – that can for many restore sound and enhance their quality of life.
Nowadays considered a fairly routine procedure, cochlear implant surgery is nevertheless complex and is becoming increasingly sophisticated. It is consequently offered only at some healthcare facilities and has recently become available to patients at Netcare Kuils River Hospital. Pieter Botha, a patient who underwent the second cochlear implant surgery at the hospital earlier this year, has found his post-operative experience of the world to be “truly remarkable”.
Performed by Dr Jaco Terblanche, an ear, nose and throat (ENT) specialist practising at the hospital, Botha underwent the operation following a serious vehicle collision in February 2020 in which he sustained severe injuries. “The accident left me with broken ribs, a broken clavicle, injured spine and head injuries that impacted my left ear. I was in the intensive care unit for eight and a half weeks and over time completely lost the hearing in my left ear, which previously had functioned completely normally.
“Dr Terblanche suggested performing the cochlear implant surgery at the time, however I had endured so much trauma from the accident and undergone so many operations and at that point, I was very hesitant about any further procedures. I tried for a year to live without hearing in my left ear but eventually I decided to proceed with the surgery. Knowing what I know now, I would never have hesitated,” says Botha.
According to Dr Terblanche, Botha was a good candidate to receive the implant, as while his cochlea had been damaged, the nerve was still intact.
A cochlear implant is a small electronic device, which helps deaf or severely hard of hearing people to recognise sounds. The device has an external component, which is usually positioned behind the ear, and an internal component that is surgically implanted into the ear. The external sound processor captures the sound before filtering and processing it and turning it into digital code. The internal implant converts the digital code into electrical impulses and sends these to an electrode array in the cochlea or inner ear. These electrodes stimulate the cochlea’s hearing nerve and send impulses to the brain where they are interpreted as sound.
“This procedure does involve some fairly detailed surgical work, as you are operating between tiny facial nerves,” says Dr Terblanche. “I am fortunate to be able to work alongside Dr Louis Hofmeyr, an ENT surgeon specialising in neurotology and otology at Netcare Christiaan Barnard Memorial Hospital.
“Dr Hofmeyr is one of the most practised specialists in South Africa when it comes to cochlear implantation, so he brings further expertise to our theatre for these procedures. It takes around three hours to complete the surgery and requires the patient to have follow-up mapping with an audiologist who makes adjustments to the implant device to get the levels right,” notes Dr Terblanche.
Botha explains that his implant is still being fine-tuned but that his hearing in the affected ear is already significantly improved and that he can take phone calls and attend virtual meetings. “The device is really very advanced and has Bluetooth capabilities, so I can not only control the volume of the device directly from my phone but am able to take calls and tune in to online meetings with the implant directly,” he says.
Cochlear implant technology has evolved significantly over time and is now at a super-sophisticated level, according to Dr Terblanche. “These implants began with just one electrode and over the past few decades have been developed to now include 14 electrodes, providing an incredibly wide range of frequencies and a much broader capability for distinguishing sounds. It is a technology that continues to be developed, and ENT specialists performing these implants are now able to take an individualised approach for each patient.
Since the first two implants at Netcare Kuils River Hospital, we now have a further four patients being assessed for cochlear implantation and we look forward to being able to make a difference in the life of many more people in the months and years to come,” says Dr Terblanche.
Dirk Truter, general manager at Netcare Kuilsriver Hospital, notes that this development will have a positive impact on people in the area seeking cochlear implantation. “It is our aim and our greatest wish to serve the communities in the vicinity of our hospital. Cochlear implants can benefit the lives of so many, from small children through to mature adults, and we are very pleased that this procedure is now available at our hospital,” concludes Truter.