“How far we have come” – the enormous evolution of cardiac surgery
Reflecting on a life-altering moment: 68-year-old Joe Jordaan from East London and renowned cardiac surgeon Dr Willie Koen photographed next to a bust of Professor Christiaan Barnard at the Netcare Christiaan Barnard Memorial Hospital, which was built in tribute to the great surgeon, whose skilled hands afforded Joe a lifetime filled with personal achievements and a loving family.
More than sixty years later, the work of Chris Barnard lives on
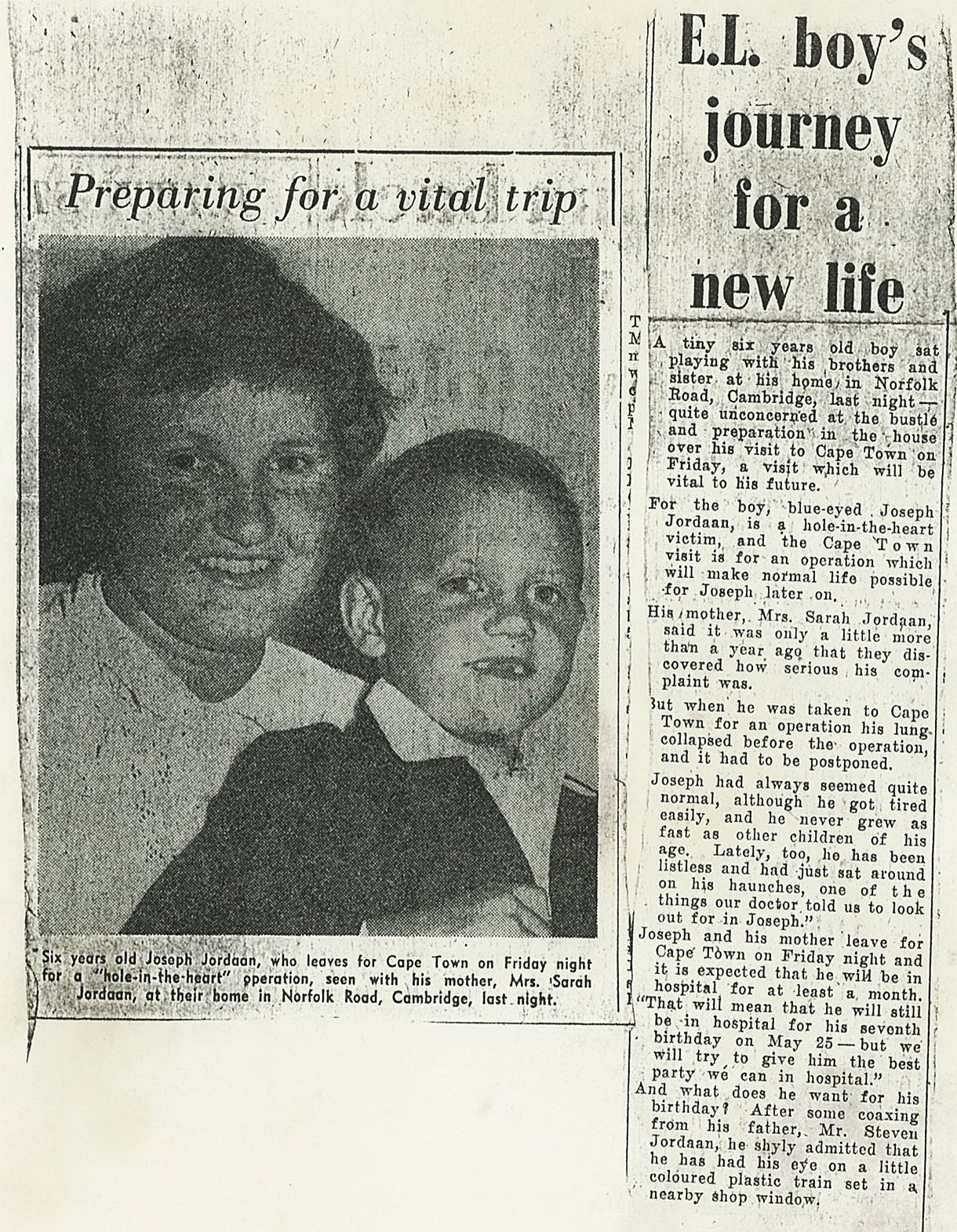
In April 1962, a six-year-old boy with a charming gap-toothed grin embarked on a life-altering journey from East London to Groote Schuur Hospital in Cape Town, a trip that would shape his destiny in a lifetime of remarkable heart health breakthroughs.
More than six decades later, Joseph Jordaan, who is now 68 years old, recently returned to the operating theatre in the Mother City, this time at the cutting-edge Netcare Christiaan Barnard Memorial Hospital, which was built in tribute to the great surgeon whose skilled hands afforded Joe a lifetime filled with personal achievements and a loving family.
Joe was born with a congenital heart defect – a condition that saw him and his mother, Sarah, make the trip to Cape Town in search of a normal life for him at a time when advances in heart surgery were limited. Little did they know that global cardiac care was on the precipice of a quantum leap.
In the same hospital where Joe’s life would be irrevocably changed, the world's first human-to-human heart transplant would be performed less than five years later on 3 December 1967 by the visionary Dr Christiaan Barnard, the very same surgeon who performed the ventricular septal defect repair to the hole in Joe’s heart.
“It was a profoundly moving moment as my colleagues and I stood in the operating theatre at Netcare Christiaan Barnard Memorial Hospital to perform Joe’s second heart procedure,” says world-renowned cardiac and transplant surgeon Dr Willie Koen.
“There was almost no evidence of the surgery performed by Professor Barnard 61 years ago to repair the hole in Joe’s heart. The work was meticulous, and to this day, it continues to serve Joe well. This time, we were working on a different heart-related modification to replace Joe’s heart valve, close to the septum where the hole in his heart had been repaired.
“It was awe-inspiring and humbling knowing that the work of this incredible surgeon – who had operated on this very same heart using very different technology more than six decades ago – lived on 22 years after he had passed on. What an incredible legacy Professor Barnard has left, not only for his patients but for surgeons like me, who were able to follow in his footsteps,” says Dr Koen.
A few days after his procedure, Joe, a retired petrol and diesel mechanic, said he was doing “one hundred per cent” well. Talking about his recent heart scare, he said, “I got such a big fright, but fortunately I got lucky a second time. A few minutes later and I would have been gone.
“My first heart procedure lasted me a lifetime, during which I married my wife Jean, and I gained three stepchildren and a daughter of my own. I was living well, eating and drinking like everyone else. Along the way I have had a few health scares which among others, resulted in having 36 centimetres of my colon removed. I also had two hip replacements. Nowadays, I watch what I eat and I don’t drink.”
For Joe’s loving wife Jean, his most recent heart procedure – which came two days before her birthday on 1 September, was an early birthday present, valuable beyond words. “We cannot wish for better,” says Joe and Jean as they count their blessings ahead of discharge and a trip back home to East London.
According to Dr Koen, ventricular septal defect repair, even by today’s standards can be a complex and difficult procedure. Back in 1962, it would take several hours, and in Joe’s case – because of complications brought on by the complexity of the procedure – it resulted in two operations of six and eight hours, respectively, in the space of a single day. Joe spent more than a month in hospital following his procedure.
At the time, repairing a hole in the heart typically involved open-heart surgery. A large incision, often in the chest area, would be made to access the heart. In some cases, a sternotomy, which involved splitting the breastbone, was necessary to gain access to the heart. To temporarily take over the heart's circulatory function, a heart-lung machine (cardiopulmonary bypass) would be connected to the patient. This machine would oxygenate the blood and pump it throughout the body while the heart was stopped.
With the heart still and blood flow diverted through the bypass machine, the surgeon would carefully locate and repair the hole in the heart using various techniques involving sutures, patches or other materials to close the hole. Once the heart was successfully repaired, the heart-lung machine would be gradually withdrawn, allowing the heart to regain its natural pumping function. The chest incision would then be closed with sutures or staples.
“It's important to note that surgical techniques and equipment have evolved significantly since 1962. Today, most heart surgeries can be performed using minimally invasive approaches, reducing the need for large incisions and the use of a heart-lung machine in some cases. Nowadays, open-heart surgeries, which are almost a routine procedure, usually require a hospital stay of four to five days. Once you're discharged from the hospital, it can take six to eight weeks for your breastbone and chest muscles to heal as you gradually return to your normal daily routine,” Dr Koen says.
“I think we underestimate the enormous evolution of cardiac surgery and how far we have come,” says Dr Koen. “It is when you look at the life of Joe Jordaan, and how he would not have seen adulthood if not for the procedure performed by Professor Chris Barnard all those years ago, and the fact that he has now been given a second lease on life once more, that you fully understand the value and tremendous impact of cardiac surgery.”